The UPA Governments list of provisions for improving the health of the population as put forth in its Common Minimum Program (CMP) was short. It promised to raise the public expenditure on health, increase investment in the control of communicable diseases, ensure healthcare for the poor through a national health insurance scheme, improve the availability of life-saving drugs at a reasonable cost and introduce a targeted population control programme in 150 districts in the country. But following criticism about its plans for a 'sharply targeted population control programme', the central government (including the Prime Minister) made repeated assertions that coercion cannot be part of any population stabilisation policy.
As a step towards fulfilling its promises, on January 4, 2005 the UPA cabinet approved the formation of a National Rural Health Mission (NRHM). The mission will aim at integrating different vertical programmes, decentralising health care service delivery at the village, and improving intersectoral action. ('Vertical' implies that machinery responsible for planning, implementing and monitoring are unique for every centrally funded program and operate without any coordination with the others. Thus when the pulse polio machinery or the HIV/AIDS machinery start rolling they do not consider the implications of such a campaign on the delivery of other health care services say maternal health or regular immunisation services.)
The bottlenecks
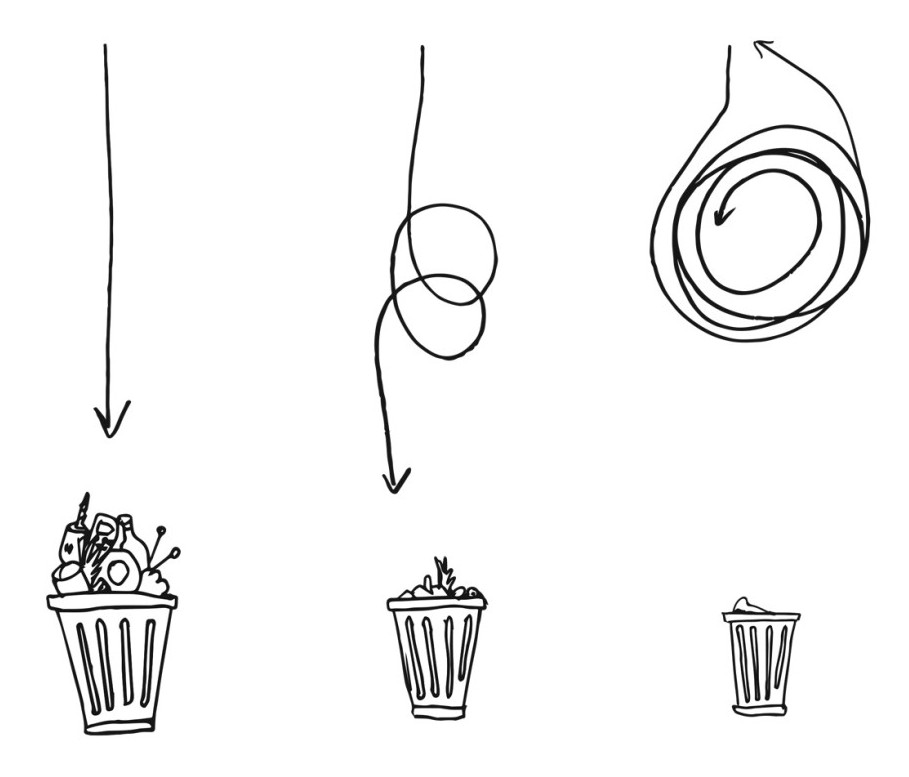
One of the main bottlenecks to the effective delivery of comprehensive healthcare services at the community level has been the multiplicity of vertical national health programmes. While all these programmes have depended upon the lowly multipurpose health worker (officially called the Auxiliary Nurse Midwife - ANM) for their implementation, the programmes' different planning, monitoring and supervisory systems bring about very uneven pattern of service delivery.
The interminable rounds of the Pulse Polio campaign have a serious impact on routine immunisation programmes as well as delivery of other essential services like maternal health. Also the family planning programme often takes precedence over all other interventions in the absence of any integrated decentralised (bottom-up) planning. The NRHM proposes to address these problems by a number of innovations at the community level.
Access at the local level
Firstly the NRHM proposes to appoint a community level health worker who has been named ASHA or Accredited Social Health Activist. It is proposed that over two hundred and fifty thousand such health workers will be appointed and they will provide first contact care to people in villages. These health workers will be women and will work closely with the Anganwadi Worker (village level worker of the Integrated Child Development Services) and the ANM. They will be chosen by and be accountable to the women in the community.
This means that women get to choose who would become the ASHA from their villages, and the ASHA would be answerable to the women as well. Health education services (covering a wide range from drinking water, sanitation, maternal and child health) would be available on a more regular basis. Health education has been a very weak point in the system currently. The ANM is either a non-resident or has too many other responsibilities (including filling up of a large number of registers, a separate one for each vertical government programme). The ASHA is also expected to provide curative assistance for fever, diarrhoea, etc.
Local priorities
A second proposal is to consolidate the different vertical programmes at the district level so that these programmes are planned and monitored through a single authority and a single district health plan. At present different programmes are supervised independently by different officers like the Deputy Chief Medical Officers, District TB Officer, District Leprosy Officer, District RCH Officer and so on. It has also been proposed in one of the planning documents that the funds available at the district will be pooled so that these can be allocated according to local priority rather than follow narrow programme lines.
There is a distinct gain from this. Planning, implementing and monitoring of specific health related activities will be done according to local priorities and not according to the nationally determined priorities of different national programmes. Thus if maternal or child health is the issue, the programmes will not be for family planning or HIV/AIDS.
More services in rural hospitals
A third and very important aspect of the proposed changes is strengthening health care delivery through rural hospitals which will provide a standardised range of services. The cabinet note mentions that 2000 such hospitals will be strengthened, while one of the earlier drafts had also mentioned that each subcentre would henceforth have two ANMs, the PHC two medical officers and the community health centre (rural hospital) 5 MBBS doctors.
The most important change that is expected from this is that specialist and surgical services will be available within the government sector (hopefully without fees or depending upon ability to pay) including emergency (obstetric) services. At present, the availability of specialist and surgical services at the rural hospital level is very low. According to a country wide facility sample survey (2000), less than 30% CHCs has an obstetrician available; less than 10% had an anaesthetist.
Local ownership of health related planning, and the monitoring of health activities by the panchayat bodies is another key area of activity proposed for the NHRM.
The NHRM promises some long awaited restructuring of the health service planning, monitoring and delivery mechanisms in the country. The first signs are promising though there was initial confusion in the thrust and approach of the mission due to the multiplicity of concept notes that emerged from the government. One of the notes in circulation, it was said, had emanated from the Prime Ministers Office, while a second was prepared by the department of family welfare.
One of the positive changes that has already come through has been the merger of the Department of Health and the Department of Family Welfare, a move formalised in early December. The bifurcation of health related activities into these two departments had for long been a sore point in the area of health related service delivery because of their competing priorities.
There is still some time before the actual mechanics of the NRHM are finalised. The success of this Mission will depend upon how some key areas are addressed and some of these are discussed below. The idea of a community health worker is very welcome but care must be taken that this person does not get converted into a local quack (informal and irrational provider). Signs of such a metamorphosis have been found in the Jan Swasthya Rakshak (JSR) scheme in Madhya Pradesh, which some say inspired the ASHA model.
Thus the ASHA worker will not only have to be provided with sufficient training, support and constant monitoring, but she will also need to be provided adequate remuneration and not be expected to survive on the basis of fees. At the same time the ASHA should not be expected to function alone but be linked up through a referral chain with the subcentre, Primary Health Centre and the Community Health Centre (rural hospital).
The referral chain of centres needs to be strengthened as well. One of the drafts being discussed had proposed that the PHC be disbanded (because doctors did not attend their posts anyway). This is a dangerous proposition and should not be allowed. Also, the Community Health Centre cannot depend only upon MBBS doctors, and at the very minimum needs a surgeon, obstetrician and anaesthetist along with blood bank facilities. This is the only way in which maternal mortality can be addressed. It is well known that maternal mortality is an enormous problem in the underserved states.
The NHRM proposes a new set of promises for the community. There have to be mechanisms which ensure that these promises are implemented in word and in spirit. Community based monitoring is essential for this to happen. The right to information campaign, the right to food campaign and the right to healthcare services campaign have amply demonstrated that given the opportunity, people are capable of understanding and monitoring government services. The role of the panchayats has to be strengthened to include other members of the community so that the programme is adequately monitored at all levels the subcentre , the primary health centre and right upto the district hospital and district health plan, and functionaries are accountable for their performance (or the lack of it).
A bold new approach like the proposed mission needs adequate financial support to ensure that all provisions are implemented. The present plan of merging the credit support and the grant-in aid to be received from different agencies like World Bank or the DFID for the Reproductive and Child Health Programme will be inadequate to fund anything substantially different from what already exists.
•
Health as an inalienable right
•
The pressure for health care
•
Elections and health
Additional budgetary provisions must be made which has already been promised in the CMP has to be harnessed for this mission. In addition to allocating extra resources a plan has to be developed which will allow each citizen of this country to access all the health services that may be necessary. The idea of universal health insurance, or targeted insurance of the poor has to be pursued with vigour.
The National Rural Health Mission has begun with great promise, now it remains to be seen whether the overall availability and quality of healthcare services for the poor and marginalised improves. Time alone will tell.