The doctors are cheerful when they walk into Pradeep Aggarwal's room. They crack jokes with the middle-aged man, who has been admitted into a posh south Delhi hospital, and tell him he is improving. But once outside his room, their faces tell a different story. They know his end is near. They feel helpless, knowing there are no medicines strong enough to help him survive.
Aggarwal has a chest infection caused by pseudomonas aeruginosa, a bacterium that has become resistant to all antibiotics.
"We feel so helpless watching such patients slide to a certain death even though modern medicine, good hospitals, good doctors and sophisticated healthcare technology are all available," says a microbiologist at the hospital. Everyday, doctors are being confronted with the growing reality that various strains of bacteria are getting tougher to kill. The World Health Organisation says that the level of resistance to drugs used to treat common infectious diseases is reaching a crisis point.
Why is this happening? Overuse and improper use of antibiotics over decades has now spawned bacteria that are immune to the drugs we have. Bacteria are microorganisms that thrive everywhere, even the cleanest of homes. They are constantly attacking our bodies, and pose the risk of causing ear infections, throat infection, tuberculosis, etc. By and large, our immune systems can fight off the bacteria. But every once in a while, the bacteria in our body reproduce faster than our immune system can kill them, and we suffer from illnesses. And we call upon a variety of drugs to restore normalcy.
Antibiotics (the term 'anti-bacterial' is often used interchangeably with 'antibiotic') were seen as miracle drugs, powerful enough to kill the harmful bacteria. But over the years, careless overuse and under use of antibiotics have helped bacteria develop immunity to powerful drugs, making them difficult or impossible to tackle. Alexander Fleming would never have imagined this, when he discovered penicillin in 1928.
Careless use of anti-biotics
Doctors all over India widely over-prescribe antibiotics, hoping for a quick definite cure apart from keeping pharmaceutical companies happy. These firms generously offer gifts and holiday trips abroad, some of them disguised as visits to attend medical conferences, to doctors who push their products. Over prescription of antibiotics ends up promoting new strains of harmful bacteria that develop immunity. "Often, doctors prescribe carelessly often succumbing to aggressive marketing and incentives offered by the drug company," says Dr. Ramachandran, of the University College of Medical Sciences in New Delhi.
At the lower levels of the pharma industry too, drugs are peddled incessantly. Just stand outside any chemist's shop, and it is quite easy to see how he plays the doctor, doling out antibiotics to patients. The drugstore clerk knows his customers are hoping to cut down on the exorbitant consultant fees of a doctor, and exploits this, assuring them that his chosen medicine is what the doctor would prescribe anyway. But, without the training and skills of a physician, these clerks make mistakes. The pills themselves are sometimes wrong, and often the dosages are excessive. And the consequences can be devastating to patients.

Doctors all over India widely over-prescribe antibiotics, hoping for a quick definite cure apart from keeping pharmaceutical companies happy. These firms generously offer gifts and holiday trips abroad, some of them disguised as visits to attend medical conferences, to doctors who push their products.
•
Sitting on an epidemic
•
Will PHFI be meaningful?
•
TB, the gravest danger
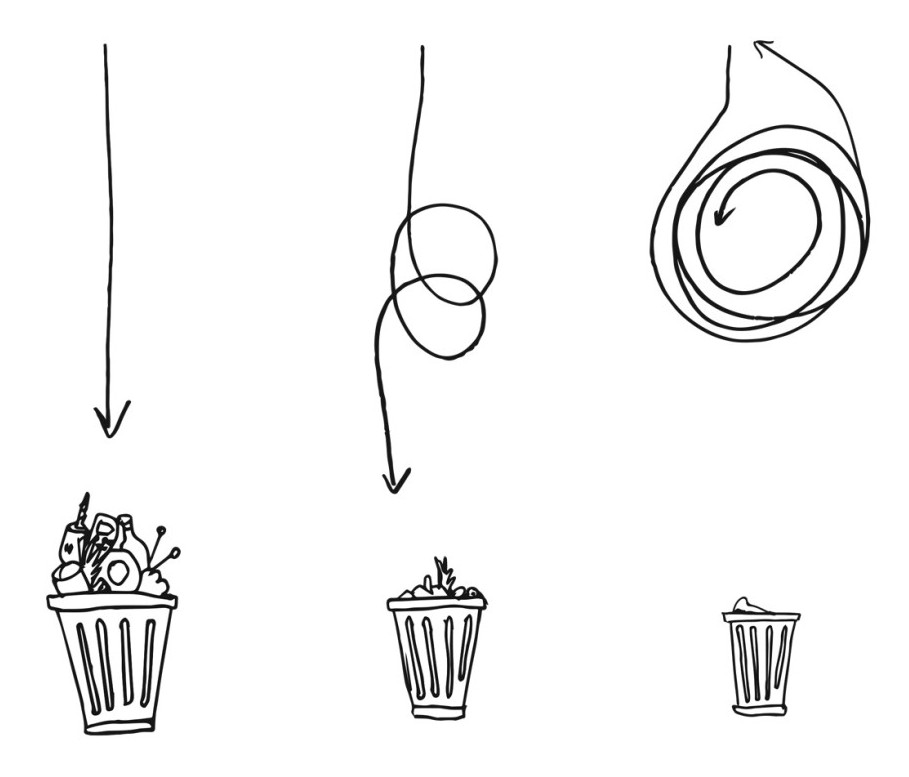
Many patients also do not complete the dosage once they feel better, hoping to save money. This helps the bacteria bounce back again after a lull, and when they return they have learnt how to deal with the antibiotic and still survive. The next time around, the antibiotic isn't good enough to tackle the tiny beast. Explains Dr. Sushma Yevale, a well known Pune gynecologist: "As many patients do not use antibiotics exactly the way they are prescribed, the bacteria progresses and rapidly grows to become resistant."
For each of us, over-prescription and incomplete use are passing acts, whose conequences are invisible. But taken as a whole, they add up to a monster we cannot control with the drugs at hand. All of us, each in our own little ways, have been cultivating Superbugs systematically for a very long time.
Alarming proportions
A survey by the World Health Organization on antibiotic use in Delhi reveals that 53 per cent of Delhiites self-prescribe antibiotics; one in four stop taking them once they feel better, instead of finishing the course; 25 per cent treat regular fever with antibiotics; and almost 18 per cent of the physicians prescribe antibiotics for non-specific fever, cough and even diarrhea. Elsewhere in India, the results are likely to be similar.
Dr. Ashutosh Shukla, Head of Internal Medicine at Artemis Health Institute, Gurgaon, says, "The emergence of Superbugs is a serious issue that needs to be immediately addressed. But it would need a lot of coordinated action from the medical fraternity and the Health Ministry to create systems to stop the over-the-counter sale of prescription drugs, and put in place a strong education campaign telling patients that overuse of antibiotics can be counter-productive and dangerous."
Dr. Shukla recently returned from a training programme at the Harvard Medical School. He found that in the out-patient department, the staff administer only the basic antibiotics and not the high end ones that doctors prescribe in India. He often finds that a lot of his patients have upper respiratory tract infections that does not require antibiotics. But most of them, he found, had already self-administered a dose of antibiotics before visiting the hospital.
Can India deal with the challenge in time?
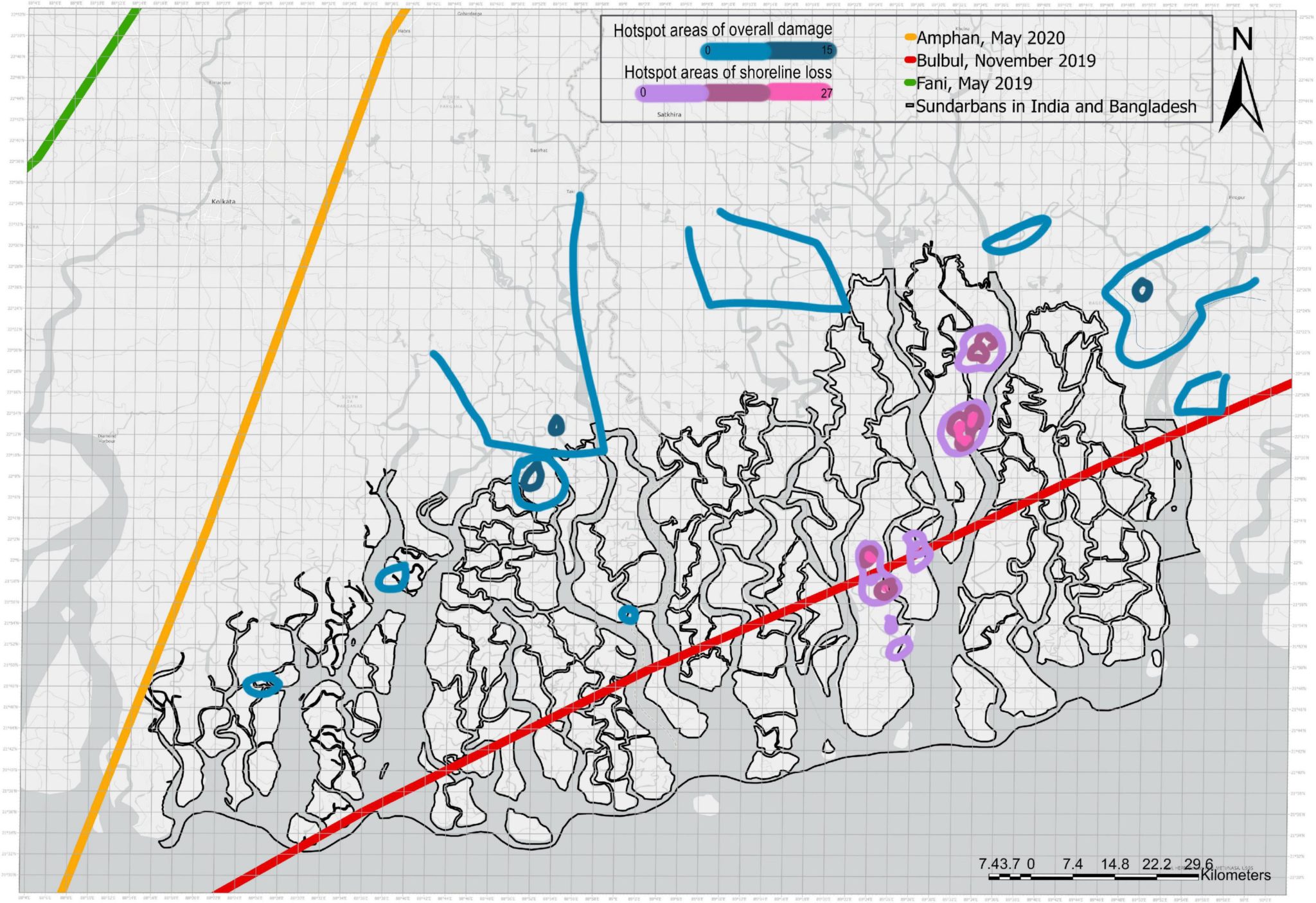
Last year, the leading medical journal Lancet ran a report claiming the presence of superbugs in New Delhi's water, calling it NDM-1. The Director General of the Indian Council of Medical Research, Dr. V M Katoch was quick to reject the report, saying that there was nothing to worry, as such organisms were found everywhere. In April this year, the Prime Minister's Office has asked for a detailed report on the issue from the Health Ministry.
Whatever this report may discover, it was troubling to note that the first respnse of the government, faced with a serious issue, is to deny it. That does not bode well for efforts to contain the potential damage.
Dr Atul Kothari, clinical microbiologist at Max Hospital in New Delhi, says that in the coming years, India may see Superbugs exploding all over. Kothari who has worked for many years both in the United Kingdom and India, says that Superbugs in the west had a low prevalence in the eighties, but in the nineties, they exponentially increased. The situation in India now is like the one that was in the west in the eighties. Doctors agree that the danger for India is real, and there is no room for complacency.
It is not just India's problem alone. Experts like the scientists at the Centers for Disease Control and Prevention in the United States say that over prescription and misuse of antibiotic drugs are the main causes of bacterial resistance. It says that up to half of the roughly 100 million prescriptions for antibiotics written each year in the United States are unnecessary!
But the developed countries are ahead on one count. The west, in particular, has woken up to this healthcare problem. It has got actively involved in tackling it. For instance, hospitals in the west are now forced by the government to publish their hospital-acquired infection rates on the web and make it available to government sources. If the hospital has a bad infection control rate, it would get less money in terms of government grants. So, there is a constant pressure to clean up, to regulate and monitor.
Besides, general practioners in developed western countries are under pressure to reduce their prescriptions of antibiotics, and this is constantly monitored. Then, there are educational programmes in schools where students are trained to tell their parents about the dangers of overusing antibiotics. This is especially helpful, as it is parents who lunge for the drugs even if the child has nothing more than a common cold. This programme has greatly helped create awareness. But nothing of this kind is happening in India.
But the situation in India is very different. There is no National Regulatory Authority in India to fix the problem of Superbugs. There is no central
body that publishes these figures. The result is that the danger spreads and no one seems to know. Warns Dr. Kothari: "If India does not recognise
increasing bacterial resistance as a problem, it will never deal with it in time."