The UPA government's National Common Minimum Programme advocates a national health insurance scheme to help the poor tide over the economic crises resulting from the costs of ill health. Is such insurance a viable option? This requires a serious national debate. Several states have been toying with such an idea of health insurance in recent months. Any hasty decisions without careful evaluation of costs and benefits will land the nation in a potentially no-win situation.
Let us look at our health crisis. First, public health expenditure in India is amongst the lowest in the world as a share of GDP, at less than 1 per cent. What is more, as a proportion of the total health expenditure, it accounts for under 20 per cent, making India a member of a small group of nations in extreme distress - like Cambodia and Afghanistan. Private health expenditure accounts for 80 per cent of the total health care costs.
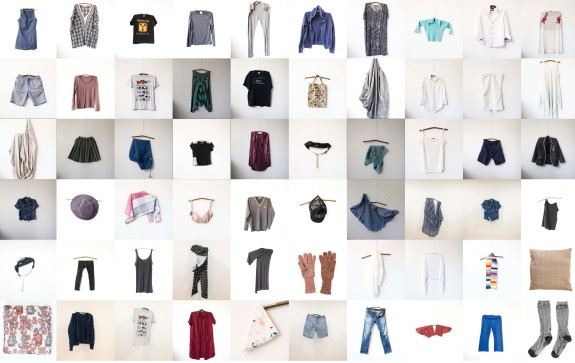
Second, most of the private expenditure is out-of-pocket (nearly 97 per cent), as there is neither health insurance coverage for the bulk of the people, nor a viable risk-pooling mechanism. As a result, the economic consequences of ill health are devastating for most families. Surveys show that a single episode of hospitalisation costs a family about 60 per cent of the annual income, on average. This high average out-of-pocket expenditure applies to all cases of hospitalisation. This is because even in public hospitals, costs are incurred for transport, accommodation and board for the patient and attendants, bribes, and often diagnostic investigations at private facilities and purchase of drugs unavailable in government hospitals. As a result, 40-60 per cent of hospitalised patients borrow heavily at high interest, and up to 30 per cent end up slipping below the poverty line on account of healthcare costs.
What a national health insurance scheme will do is simply transfer these costs to the public exchequer. The experience of many health insurance projects run by civil society initiatives and non-profit foundations indicates that the average actuarial costs even for a modest health insurance coverage will be about Rs 300 per capita per annum. A national scheme would involve coverage of about 300 million poor people with full government subsidy, and another 400 million lower middle-class people with 50 per cent subsidy. The cost to the exchequer will be around Rs 15,000 crores per annum for any credible national insurance programme, even with modest and limited risk coverage. When the current public health expenditure is only Rs 25,000 crores, a 60 per cent escalation only for health insurance is unrealistic and unsustainable. Such shift in expenditure will actually result in subsidising private hospitals.
Worse, such a diversion of expenditure could further diminish resources for preventive and public health. Most of the disease burden is a consequence of primary care failure. The need of the hour is clearly to strengthen preventive and public health systems to obtain best value for the money spent, reduce the disease burden and promote overall health. Excessive reliance on health insurance as a means of healthcare delivery is neither prudent nor cost effective. Health insurance will only address the symptoms of public health failure, without reducing the disease burden. This failure of preventive health will only escalate costs of curative medicine, in the fond hope that more hospitals will ensure better health.
Furthermore, insurance usually involves adverse selection of beneficiaries, as those who are likely to benefit from hospital care are more likely to join it. There is also the moral hazard problem of two kindsâpoor hospital care once the population is enrolled in the risk-pooling mechanism, and over-consumption of medical services by the richer and better-informed sections. As a result, in OECD countries, healthcare costs are growing much faster than GDP. The total healthcare costs in rich countries are estimated at an astronomical $3 trillion. Let us not repeat the mistakes of other countries.
The range of diseases is also changing slowly in India with enhanced prosperity, better preventive care and longer life spans. India should therefore move towards risk-pooling options to reduce the burden of hospital costs on individual patients. But our first priority should be improvement of public health delivery systems. That is where the least investment yields the best returns. Meanwhile, the government can encourage the innovative schemes taken up by credible institutions such as SEWA in Ahmedabad or Tribhuvandas Foundation in Gujarat. Subsidies to such schemes may work.
Instead of going for what look like obvious solutions but are actually riddled with problems, India needs to devise risk-pooling schemes primarily involving public sector institutions. In a scheme where money follows the patient and public hospitals are rewarded on the basis of services delivered, the incentives will be dramatically altered, and service will improve. Such risk-pooling will strengthen public sector while providing relief for the poor.